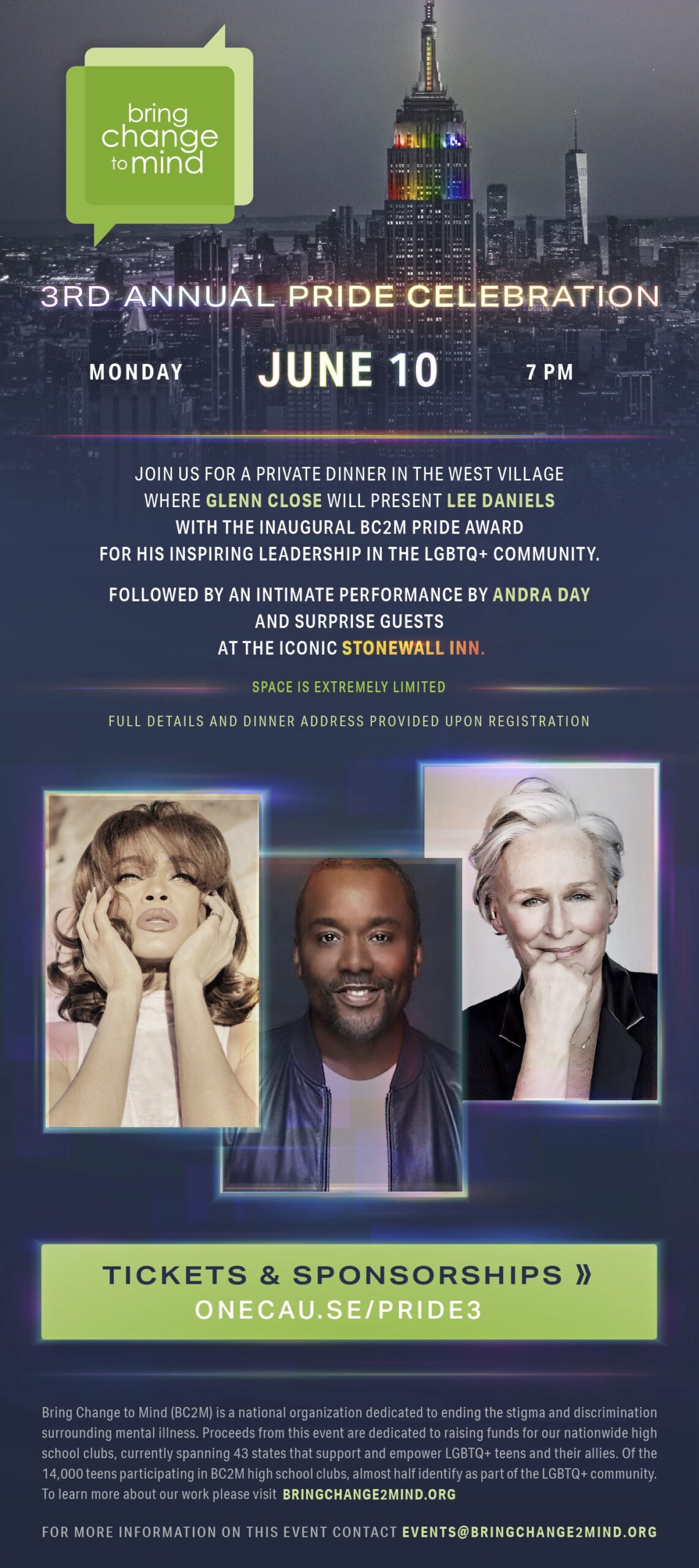
Digital & IRL Resources
Whether it’s for yourself or for a friend or family member, checking in on one’s mental health is always a good idea—and we’ve got the tools to help. Keep scrolling to learn more.


Choose Your Words
Talking to a friend? A parent? A teacher? A student? Here’s how.
(Spoiler alert: it’s often easier than you think.)

Talk to a Friend
I support you no matter what.
I noticed you aren’t acting like yourself lately.
You are not a burden.

Talk to an Adult
You are not alone.
What can I do to help?
I am here to listen.

Talk to a Young Adult
I am not feeling like myself.
I feel like things are out of control and I’m not sure how to keep myself together.
You don’t have to solve it for me. I just need you to listen.

Talk About Yourself
I’ve been feeling off. Have a minute?
I’m not thinking clearly these days. Can we talk?
I feel really alone and need help.
Say This, Not That
Words matter—especially the ones we don’t realize we’re saying.
Click the cards below to flip them over for a better way of talking about mental health.
Instead of
saying:
She suffers from mental illness.
Say this:
She lives with mental illness.
Instead of
saying:
That is so crazy!
Say this:
That is so surprising!
Instead of
saying:
You’ll get over it eventually. Just cheer up!
Say this:
I’m here to listen if you want to talk.
Instead of
saying:
It can’t be that bad.
Say this:
I believe you.
Instead of
saying:
He’s bipolar.
Say this:
He lives with bipolar disorder.
Instead of
saying:
Just get over it already.
Say this:
Can you tell me more about what you’re going through?
Instead of
saying:
Stop being lazy.
Say this:
How can I make things easier for you?
Instead of
saying:
Why can’t you just be normal?
Say this:
I admire your strength.

PepTalk
There are people like you all around the world. Feeling the same feelings, thinking the same thoughts. Don’t believe us? Click below to check out our PepTalk tool, to give or get words of encouragement.
Talk Tool
Finding the right words, no matter what you’re feeling or what side of the conversation you’re on, can be difficult. So we made a handy dandy tool to help get the conversation started.

Blog
Sometimes, the best way to help yourself or another is to listen. Or, in this case, read. Check out our Blogs to read articles written by BC2M Ambassadors and featured Guest Writers.
Take A Break
Follow this guided visual meditation to help focus your attention, clear your mind, and just breathe.

Understanding
Mental Illness
Mental illness is a disorder of the brain that can happen to anyone, and can be caused by a variety of different sources—from genetics to other biological, environmental, and social/cultural factors. It’s no one’s fault. It’s not “weird” or abnormal. But it can be difficult to understand. Click through the cards below to start learning more about specific mental health terms.
Attention Deficit Hyperactivity Disorder (ADHD) is a chronic condition that affects millions of children and often persists into adulthood. People with ADHD could have difficulty paying attention, following through on instruction, and staying organized.
The difference between occasional anxiety and anxiety disorders is that occasional anxiety usually involves temporary worry or fear, while anxiety disorders are characterized by anxiety, worry, or fear that interferes with everyday activities.
People living with Bipolar Disorder experience more severe symptoms than the normal “ups and downs” we go through every now and then. Also known as manic-depressive illness, Bipolar Disorder causes unusual shifts in mood, energy, activity levels, and the ability to carry out day-to-day tasks.
People living with Borderline Personality Disorder (BPD) can have problems regulating emotions and thoughts, impulsive and reckless behavior, and unstable relationships with others.
Depression is a common medical condition that adversely affects how you feel, think, and act. Depression is not a poor reflection of character, upbringing, or capabilities.
People with Dissociative Identity Disorder (DID) experience a disconnection and lack of continuity between thoughts, memories, surrounding, actions, and identity that are involuntary and unhealthy.
Eating Disorders can cause people to become so preoccupied with food and weight that he or she can often focus on little else, leading to serious physical problems.
Obsessive Compulsive Disorder (OCD) drives people to perform compulsive acts led by unreasonable thoughts and fears (obsessions) that lead to repetitive behaviors (compulsions). It is possible to have only obsessions or only compulsions and still have OCD.
Post-Traumatic Stress Disorder (PTSD) is an anxiety disorder that can develop after experiencing a traumatic event or ordeal in which physical, psychological, or sexual harm occurred or was threatened. People who have PTSD may feel stressed or frightened even when they’re no longer in danger.
Schizophrenia is a chronic and severe mental disorder that affects how a person thinks, feels, and behaves. People living with schizophrenia may experience symptoms including delusions, hallucinations, and major episodes of mood instability.

Additional Resources
Looking for more ways to help yourself or another? Take a look at the categories below to find a list of links to get you started in the right direction.